Search
Citas y referencias (14)
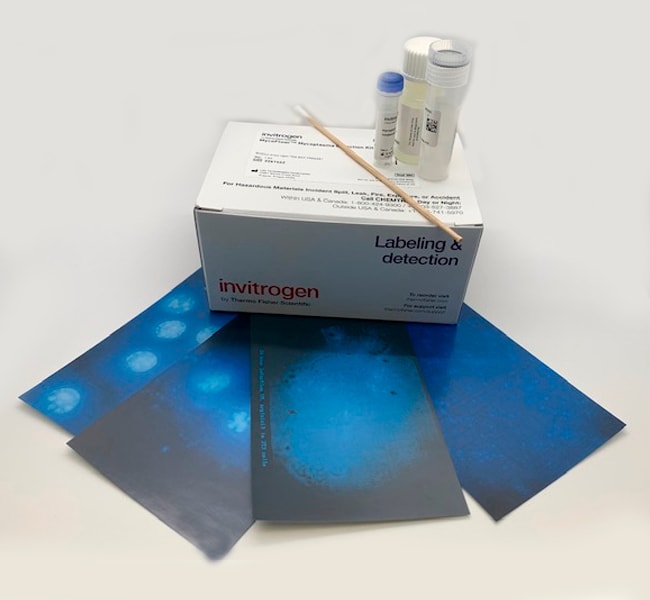
Invitrogen™
MycoFluor™ Mycoplasma Detection Kit
El kit de detección de micoplasma MycoFluor™ proporciona un ensayo microscópico de fluorescencia ultrasensible, rápido y simple para la identificaciónMás información
| Número de catálogo | Cantidad |
|---|---|
| M7006 | 100 pruebas |
Número de catálogo M7006
Precio (USD)
675,54
Each
Cantidad:
100 pruebas
Precio (USD)
675,54
Each
El kit de detección de micoplasma MycoFluor™ proporciona un ensayo microscópico de fluorescencia ultrasensible, rápido y simple para la identificación visual de la infección por micoplasma en cultivos celulares de laboratorio. Para detectar micoplasma, el reactivo fluorescente MycoFluor™ se añade directamente al medio de cultivo, con o sin células, y la muestra teñida se examina bajo un microscopio de fluorescencia.
Para uso exclusivo en investigación. No apto para uso en procedimientos diagnósticos.
Especificaciones
Método de detecciónFluorescente, Fluorescente
Para utilizar conMicroscopio de fluorescencia
Cantidad100 pruebas
Condiciones de envíoTemperatura ambiente, Temperatura ambiente
FormularioLíquido
Tipo de productoDetección de micoplasma
Unit SizeEach
Contenido y almacenamiento
Almacenar en el refrigerador (2–8 °C) y proteger de la luz.
Preguntas frecuentes
I suspect mycoplasma is affecting the growth rate of my culture. How can I test for it?
Which fluorescence filter should I use with the MycoFluor Mycoplasma Detection Kit (Cat. No. M7006)?
Can I develop the MycoFluor MycoPlasma Detection Kit (Cat.No. M7006) into a 96-well format for screening with a plate reader?
How can I remove mycoplasma contamination from my cell culture medium?
Citations & References (14)
Citations & References
Abstract
Characterization of a novel epigenetic effect of ionizing radiation: the death-inducing effect.
Journal:Cancer Res
PubMed ID:12543783
'The detrimental effects associated with exposure to ionizing radiation have long been thought to result from the direct targeting of the nucleus leading to DNA damage; however, the emergence of concepts such as radiation-induced genomic instability and bystander effects have challenged this dogma. After cellular exposure to ionizing radiation, we
Mechanisms of cell death associated with death-inducing factors from genomically unstable cell lines.
Journal:Mutagenesis
PubMed ID:14614192
'We recently described a unique non-targeted effect of ionizing radiation whereby growth medium from two clones of GM10115 cells exhibiting radiation-induced chromosomal instability was cytotoxic to parental GM10115 cells. We termed this the death-inducing effect (DIE). The goal of the present study was to determine how DIE killed cells. Our
Ionizing radiation induces delayed hyperrecombination in Mammalian cells.
Journal:Mol Cell Biol
PubMed ID:15143196
Exposure to ionizing radiation can result in delayed effects that can be detected in the progeny of an irradiated cell multiple generations after the initial exposure. These effects are described under the rubric of radiation-induced genomic instability and encompass multiple genotoxic endpoints. We have developed a green fluorescence protein (GFP)-based
Angiotensin subtype 1 rReceptor (AT1) blockade improves vasorelaxation in heart failure by up-regulation of endothelial nitric-oxide synthase via activation of the AT2 receptor.
Journal:J Pharmacol Exp Ther
PubMed ID:14560036
To determine whether angiotensin receptor blockade decreases vascular tone in heart failure by improving endothelial-dependent vasorelaxation and increasing nitric oxide (NO) bioavailability, we treated infarcted adult male Sprague-Dawley rats with candesartan for 7 days or 8 weeks (10 mg/kg/day in drinking water). Candesartan, at both time points, lowered left ventricular
Combination therapy of BCR-ABL-positive B cell acute lymphoblastic leukemia by tyrosine kinase inhibitor dasatinib and c-JUN N-terminal kinase inhibition.
Journal:J Hematol Oncol
PubMed ID:32552902