 According to virologists and epidemiologists, the Delta variant is the fastest, fittest, and most formidable version of Coronavirus the world has encountered. Delta seems to carry an increased risk of hospitalization. Delta seems to be much more transmissible than previous forms of the virus and is comparable to chickenpox. Vaccinated people can still be infected by Delta and can transmit it to others.1
According to virologists and epidemiologists, the Delta variant is the fastest, fittest, and most formidable version of Coronavirus the world has encountered. Delta seems to carry an increased risk of hospitalization. Delta seems to be much more transmissible than previous forms of the virus and is comparable to chickenpox. Vaccinated people can still be infected by Delta and can transmit it to others.1
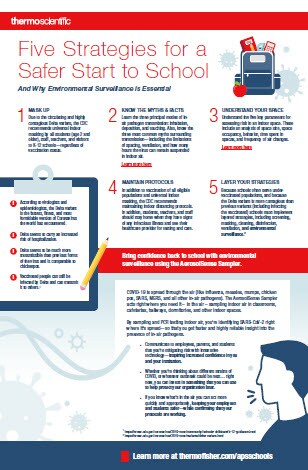
School administrators are concerned and wondering how they can bring confidence back to school. Here are five strategies to a safer start to school.
- MASK UP
Due to the circulating and highly contagious Delta variant, the CDC recommends universal indoor masking by all students (age 2 and older), staff, teachers, and visitors to K-12 schools—regardless of vaccination status. - KNOW THE MYTHS & FACTS
Learn the three principal modes of in-air pathogen transmission: inhalation, deposition, and touching. Also, know the three most common myths surrounding transmission—including the limitations of spacing, ventilation, and how many hours the virus can remain suspended in indoor air. (Learn more here) - UNDERSTAND YOUR SPACE
Understand the five key parameters for assessing risk in an indoor space. These include an analysis of space size, space occupancy, behavior, time spent in spaces, and frequency of air changes. Here are five questions you should ask when assessing in-air pathogens transmission indoors: - What size is the space? Once infectious droplets and particles are exhaled, they move outward. Thus, the risk for infection increases with proximity and decreases with distance – corresponding with square footage of an indoor space.
- How many people are in the space? Once you know the size of an indoor space, consider the number of potentially infectious people within. The more people in a space, the greater the risk of airborne pathogen transmission.
- How are the people behaving in the space? Are people in the space exercising? Singing? Laughing? Wearing masks? Behavior will affect in-air pathogen transmission – both increasing the likelihood of in-air pathogens being inhaled and exhaled.2
- How long are individuals occupying the space? Another crucial consideration is the duration people spend within a space. The more time people spend in a space, the more potential exposure they have to in-air pathogens. And the less time they spend in a space, the less their potential exposure.
- How often is the air in the space “changed?” The final factor to consider while assessing the risk of in-air pathogen transmission is new air changes. How frequently is the air in a space rotated (or changed) with new air? While the standards for adequate ventilation are stringent, in-air pathogen risk will correlate directly to the frequency of new air changes.3,4
- MAINTAIN PROTOCOLS
In addition to vaccination of all eligible populations and universal indoor masking, the CDC recommends maintaining indoor distancing protocols. In addition, students, teachers, and staff should stay home when they have signs of any infectious illness and see their healthcare provider for testing and care. - LAYER YOUR STRATEGIES
Because schools often serve under-vaccinated populations, and because the Delta variant is more contagious than previous variants (including infecting the vaccinated) schools must implement layered strategies, including screening, masking, cleaning, disinfection, ventilation, and environmental surveillance.2
Environmental surveillance technology is essential as it acts right where you need it – in the air – sampling indoor air in classrooms, cafeterias, hallways, dormitories, and other indoor spaces. By sampling and PCR testing indoor air, you’re identifying SARS-CoV-2 right where it’s spread—so that you get faster and highly reliable insight into the presence of in-air pathogens.
If you know what’s in the air you can act more quickly and appropriately, keeping your employees and students safer—while confirming that your protocols are working. Environmental and occupational surveillance with air sampling complements the insight you already gain from individual testing, enabling you to better assess the safety of air quality within facilities for communities.
You can download a copy of these 5 strategies
Resources:
1 https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html,
2 https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html,
3 https://www.medrxiv.org/content/10.1101/2021.03.17.21253800v1.full-text,
4 https://www.nature.com/articles/d41586-021-00810-9#ref-CR3 with environmental surveillance using the AerosolSense Sampler.






Leave a Reply